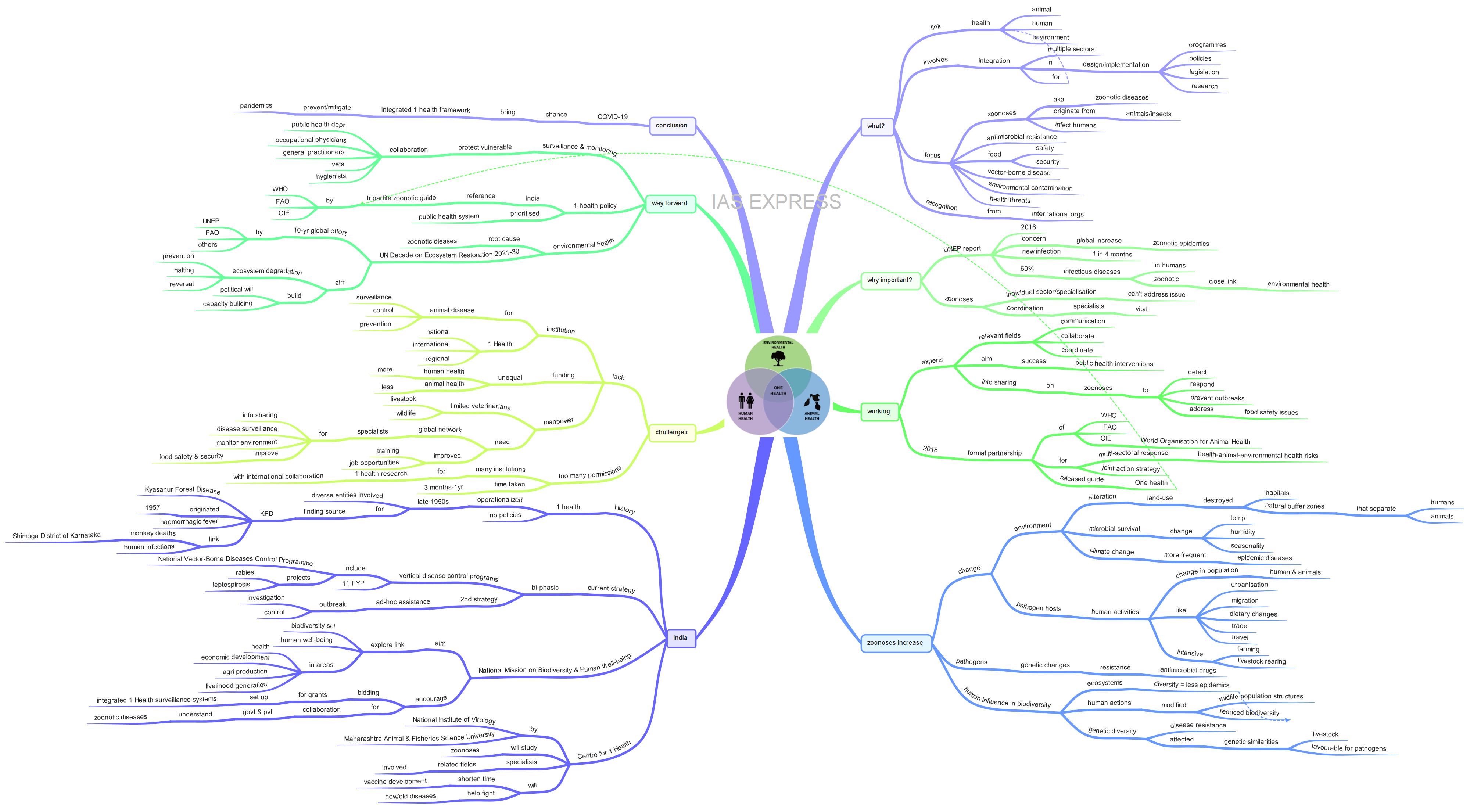
One Health Approach – Need, Opportunities, Challenges

Rudolf Virchow, the father of pathology, had once said, “Between animal and human medicine, there are no dividing lines – nor should there be”. This holds true especially in recent years with the increase in the instances of epidemic outbreaks due to zoonoses. This calls for the use of One Health approach, a paradigm shift in the human and animal health along with the conservation of biodiversity to ensure prevention and mitigation of pandemics like that of COVID-19.
This topic of “One Health Approach – Need, Opportunities, Challenges” is important from the perspective of the UPSC IAS Examination, which falls under General Studies Portion.
What is One Health approach?
- Human, animal and environmental health are inseparably linked.
- One health approach recognises this and it aims to integrate efforts in medicine, veterinary medicine, public health, agriculture and environmental health.
- It involves designing and implementing programmes, policies, legislation and research in which multiple sectors communicate and work together to achieve better health outcomes.
- The areas of work in which the One Health approach is particularly relevant are zoonotic diseases, antimicrobial resistance, food safety and security, vector-borne disease, environmental contamination and other health threats shared by people, animals, and the environment.
- International organisations like World Bank, World Health Organisation (WHO), Food and Agriculture Organisation (FAO), World Organisation for Animal Health (OIE), United Nations System Influenza Coordination (UNSIC) etc., have recognised this approach as one of the efficient means to address the issue of epidemics in the future.
Why has One Health approach gained prominence in recent years?
- In 2016, the United Nations Environment Programme (UNEP), through a report, highlighted a worldwide increase in the zoonotic epidemics as an issue of concern.
- According to the report, one new infectious disease emerges in humans every four months.
- Specifically, it pointed out that 60% of all emerging infectious diseases in humans are zoonotic and that these diseases are closely linked with the health of ecosystems.
- Zoonotic diseases or zoonoses are diseases that originate from animals or insects to infect humans. These diseases are caused by virus, bacteria, fungus and parasites.
- Examples for zoonotic diseases include Rabies, Salmonella infection, Anthrax, Brucellosis, Ebola etc.
- As zoonoses infect both animals and humans alike, one sector alone cannot address the problem.
- For instance, rabies in humans can be prevented by targeting the animal source of the virus, like vaccinating the dogs.
- Information on influenza virus circulating in animals is vital to the selection of viruses for human vaccines for potential influenza pandemics.
- Thus, coordination among the experts in these individual fields is vital to address these issues.
How does One Health approach work?
- In this approach, experts in human, animal, environmental, health and other relevant disciplines and sectors are involved in monitoring and controlling public health threats and learning how diseases spread among people, animals, plants and the environment.
- Professionals in human health (doctors, nurses, public health practitioners, and epidemiologists), animal health (veterinarians, paraprofessionals, and agricultural workers), environment health (ecologists and wildlife experts) and other areas of expertise communicate, collaborate and coordinate to ensure successful public health interventions.
- Additionally, law enforcement, policymakers, agriculture, communities and even pet owners play a critical role in this approach.
- By promoting collaboration among these people, One Health approach aims to achieve the best health outcomes for people, animals and plants in a shared environment.
- Through effective collaboration, epidemiological and laboratory information are shared across sectors, government officials, researchers etc., to effectively detect, respond to and prevent outbreaks of zoonoses and food safety issues.
- In this context, WHO works alongside FAO and OIE to promote multi-sectoral response to food safety hazards, zoonoses and other public threats and provide guidelines to reduce these threats.
- On May 2018, these organisations have consolidated a formal partnership to combat health-animal-environmental health risks and to strengthen joint action strategy.
- A year later, due to this partnership, they released a guide that provides principles and best practices to aid countries in achieving sustainable and functional collaboration at the human-animal-environment interface.
Why is there an increase in the occurrences of zoonotic diseases in recent years?
Environmental changes:
- Human activities have led to major changes in the environment.
- By altering land use, for settlement, agriculture, extractive and other industries and their associate infrastructure, humans have encroached and destroyed animal habitats.
- This led to the destruction of the natural buffer zones that would normally separate humans from animals, creating opportunities for zoonoses to spillover from wild animals to people.
- Climate change, which is mainly caused by greenhouse gas emission, has worsened the situation.
- Changes in temperature, humidity and seasonality directly affect the survival of microbes in the environment.
- Evidence indicates that epidemic diseases will become more frequent as the climate continues to change.
Changes in pathogen hosts:
- Changes in human and animal populations, which serve as hosts for certain pathogens, are mostly due to human activities.
- Migration, urbanisation, changing dietary practices, trade and travel are some of the causes for these changes.
- In many developing countries, economic growth and demographic shift from rural to urban areas have increased consumer demands for dairy and meat products in cities.
- This resulted in the expansion of cropland and more intense livestock farming near and around cities, increasing opportunities for exposure to pathogens.
- Livestock often serves as an epidemiological bridge between wildlife and human infections, like in the case of avian influenza and coronavirus.
- Proximity to different species via wet market or consumptions of wild animals can also facilitate animal to human transmission.
- The on-going pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is said to have originated from the city of Wuhan in China, from a wet market of live animals.
- Globalisation also plays a major role in spreading infections across the world.
Changes in pathogens:
- Pathogens undergo genetic changes (mutates), allowing them to survive in new environments.
- Example: resistance of pathogens to antimicrobial drugs (antibiotics, antifungals, antiretrovirals and antimalarials).
Human influence in biodiversity:
- Ecosystems are innately resilient and adaptable, enabling them to support diverse species and regulate diseases.
- The more diverse an ecosystem is, the more difficult it is for one pathogen to spread rapidly or dominate.
- However, human actions have modified wildlife population structures and reduced biodiversity at an abnormal rate, producing favourable conditions for particular hosts, vectors and/or pathogens.
- Genetic diversity provides a natural source of disease resistance among the animal population.
- However, intensive livestock rearing often produces genetic similarities within herds and folks, making them more susceptible to pathogens to spread from wild animals to humans.
- Similarly, diverse areas enable disease-transmitting vectors to feed on a larger variety of hosts, some of which cannot support these pathogens.
- In contrast, when pathogens occur in less biodiverse areas, transmission can be amplified exponentially.
How is the concept of One Health approach used in India?
History:
- Although the concept of One Health emerged relatively recently, it was operationalized in India in the late 1950s.
- It helped in the discovery of the source of Kyasanur Forest Disease (KFD), a highly dangerous haemorrhagic fever that is more deadly than COVID-19.
- It was locally called “monkey fever” because of the link between the deaths of monkeys and human infection in Shimoga District of Karnataka where it originated in 1957.
- The diverse entities like Rockefeller Foundations, Pune-based National Institute of Virology, World Health Organisation (WHO) and the Bombay Natural History Society came together to deal with this crisis.
- While the Rockefeller Foundation provided financial and technical assistance, researchers from Virus Research Centre surveyed the Western Ghats forest for potential carriers and conducted autopsies on monkeys in their investigation into the cause of the disease.
- Even research to eliminate the possibility of the disease caused by migratory birds was undertaken.
- Though this combined efforts of these entities led to success, it largely remains an isolated example.
- This did not lead to similar research and integration of the same method in the public health system to combat zoonotic diseases.
- India is yet to have a national One Health policy.
Strategy for Zoonosis:
- Currently, India’s disease control mechanism is bi-phasic.
- It includes vertical disease control programs like National Vector-Borne Diseases Control Programme, projects for rabies and leptospirosis control. These programmes have been incorporated in the 11th Five Year Plan (2007-08).
- The second strategy includes the provision of ad-hoc assistance for outbreak investigations and control.
- As of now, India’s response is mostly reactive, lacking solid One Health Framework.
National Mission on Biodiversity and Human Well-being:
- The country has recently launched the National Mission on Biodiversity and Human Well-being.
- It aims to explore the links between biodiversity science and human well-being across the sectors of health, economic development, agricultural production and livelihood generation in combination with efforts to mitigate climate change and related issues.
- One of the components of this mission explicitly links biodiversity to human health through One Health Framework.
- This programme encourages bidding among institutions for grants to set up integrated One Health surveillance systems across India at 25 sentinel surveillance sites in potential emerging infectious disease hotspots.
- In this manner, government and private institutions of varying disciplines can collaborate to understand zoonotic diseases’ origin, threats and spreading so that they can be dealt with promptly.
Centre for One Health:
- The National Institute of Virology (NIV) and Maharashtra Animal and Fisheries Science University (MAFSU), Nagpur, are currently setting up Centre for One Health to help the country be better prepared for future epidemics.
- This Centre will study the different diseases caused by pathogens in domestic and wild animals.
- Veterinarians, environmental scientists and medical scientists will be involved for this purpose.
- The research under the umbrella of One Health Centre will shorten the time taken to develop vaccines.
- This will not only help India combat the new and unknown diseases but also for eradicating existing dangerous diseases like tuberculosis, which India aims to eradicate by 2030.
- This Centre is also going to have a Bio Safety Lab (BSL)-4 Lab, which is vital for handling hazardous pathogens.
What are the challenges?
- Institutions: Many countries do not have institutions whose primary missions are animal disease surveillance, control and prevention. Creation of One Health Organisations at the international, national, regional and local levels with integrated missions to improve human, animal and environmental health can improve global health while preventing and controlling infectious diseases.
- Funding: Currently, human health is better funded than animal health (some countries have minimal or no veterinary medicine). More funding must be provided to address this issue.
- Manpower: Currently, very few veterinarians are pursuing careers in livestock and wildlife health, probably due to limited job opportunities in this field. More veterinary schools must be created at the domestic and global levels. For the One Health approach to succeed, a global network of qualified individuals working locally, regionally, nationally and internationally must be created to share information, conduct disease surveillance in the human and animal population, monitor environment and improve food safety and security. They must be educated, trained and provided with job opportunities in the vital fields like animal epidemiology, livestock and wildlife health etc.
- Too many permissions: The regulatory framework for doing One Health research in India with international collaboration requires approval from multiple authorities, including ICMR, various union ministries, Director General of the Armed Forces, National Biodiversity Authority, Committee of the Purpose of Control & Supervision of Experiments on Animals, state health authorities etc. Additional permissions are also required from state forest authorities and biodiversity boards for accessing biological resources within natural landscapes. There is also the issue of long waiting periods (3 months to one year). This hampers the ability to rapidly respond to emerging threats from infectious diseases.
What can be the way forward?
Monitoring & Surveillance:
- Apart from addressing the aforementioned key challenges, the One Health Approach requires monitoring and surveillance.
- Those having greater exposure to zoonotic disease than others do, like farmers or butchers, are the most vulnerable to these diseases and they require more attention.
- The public health departments must collaborate with hygienists, occupational physicians, general practitioners and veterinarians to to jointly monitor the health of vulnerable communities, animals and the general population.
National-level One Health Policy:
- The Indian government must create an individual national One Health policy with reference to the tripartite zoonotic guide framed by WHO, FAO and OIE.
- One Health approach must also be prioritised in the public health systems, both at the national and international levels.
Safeguarding environmental health:
- The zoonotic diseases require addressing of the root cause, mainly the impact of human activities on the ecosystem.
- This means monitoring of human and wildlife health in landscapes for improving the understanding and preparedness for potential zoonotic outbreaks.
- As the global population increases and expands, there is a need for a fundamental reshaping of the human relationship with nature.
- Therefore, UNEP, FAO and other organisations are launching a 10-year effort called the UN Decade on Ecosystem Restoration 2021-30 to prevent, halt and reverse the degradation of the ecosystem.
- This is a globally coordinated effort to address the loss and degradation of habitats.
- It focuses on building political will and capacity to restore habitats.
Conclusion:
With the human population ever-increasing, there is an increase in the chances of pandemics like that of COVID-19 in the future. This situation gives India and the world a huge opportunity to bring forth an integrated One Health framework to prevent the repetition of the same.
Practice question for mains:
Caring for animal and environmental health plays a pivotal role in human health and welfare. Elucidate. (250 words)